The productivity report gives the user a high-level glance at charges, payments, and adjustments based upon a selected date range, provider, and supervisee. This document walks through the process of accessing and producing a productivity report, as well as explains the information it presents.
Navigate to Reports | System Reports | select Productivity from Billing drop down menu
Report Instructions
- Enter a beginning date in the start date field in MM/DD/CCYY format. Users can also click the calendar icon to select a date from the calendar tool. The report will include any data between the date you specify and the current date.
- Select a provider from the "Provider" drop-down. Users may specify one provider from the list, or select the "ALL PROVIDERS" option located at the top. The report will be built upon the provider(s) you choose.
- Select a supervisee the exact same way using the "Supervisee" drop-down.
- Click Preview to generate the report.
Field Definitions
- Start Date – The beginning date of the report. The productivity report will account for all the data between the date entered and the current date.
- Provider Drop-Down – The provider upon which the productivity report is built. The user can select an individual provider from the drop-down list, or select the "ALL PROVIDERS" option located at the top.
- Supervisee Drop-Down – The supervisee upon which the productivity report is built. The user can select an individual supervisee from the drop-down list, or select the "ALL SUPERVISEES" option located at the top.
- Preview Button – Creates a preview of the report based upon the specified start date, provider, and supervisee. If any of the fields are missing a valid entry, this button will be grayed out.
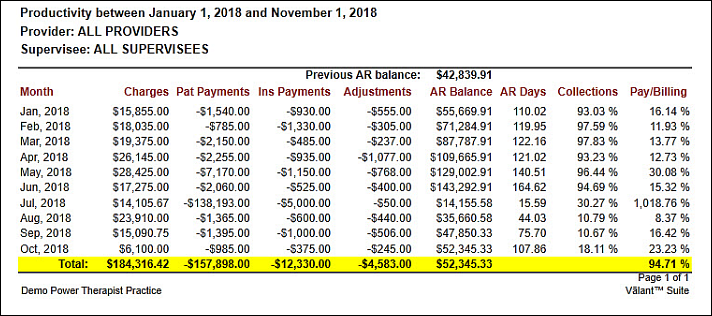
Column Definitions
- Month – The month and year from which the data was retrieved.
- Charges – The total amount of charges accrued for the listed month.
- Pat Payments – The total amount of patient payments received for the listed month.
- Ins Payments – The total amount of insurance payments received for the listed month.
- Adjustments – The total amount of adjustments made for the listed month.
- AR Balance – The running total of all outstanding accounts receivable balances.
-
AR Days– The number of days that customer invoices are outstanding before payments are collected, in order to give an understanding of the overall effectiveness of collection efforts.
- The calculation is as follows: (AR Balance for the month * Inclusive number of days in the last four months) / (Inclusive charges in the last four months)
-
Collections– The percentage of the charges for the listed month that have been settled. This percentage does not take adjustments into consideration – only patient and insurance payments.
- The calculation is as follows: (Patient Payments + Insurance Payments) / (Charges)
-
Pay/Billing– The percentage of the billing for the listed month that has been settled. This percentage takes adjustments into consideration, in addition to the usual patient and insurance payments.
- The calculation is as follows: (Patient Payments + Insurance Payments) / (Charges – Adjustments)