In order to create an insurance claim for primary insurance, complete the following steps:
Navigate to Billing | Create Insurance Claims
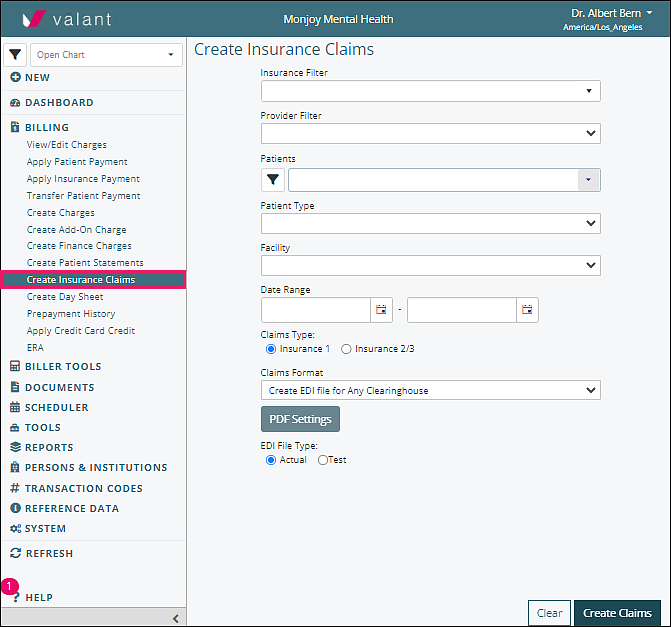
In order to submit all outstanding claims, all of the fields should be left blank. Pick the type of claims format needed. Selecting “Submit automatic EDI file...” from the Claims Format drop-down list transmits claims directly to the clearinghouse.
Click Create Claims
Once this is completed please follow the same steps to submit claims to all secondary and tertiary insurance after selecting the appropriate Claims Type radio button.
Filters
Individual claims can be created by using the filter functions to create the desired claims.
- Insurance Filter: allows you to create insurance claims for one or all insurance companies except for one
- Provider Filter: allows you to create insurance claims for one or all providers except for one
- Patients Filter: allows you to create insurance claims for one or all patients except for one
- Patient Type: allows you to create insurance claims for one or all patient types except for one
- Facility: allows you to create insurance claims for one or all facilities except for one
- Date Range Fields: allows you to create insurance claims for services that fall only within the selected date range
- Claims Type Radio Buttons: chooses if claims are being generated for primary or secondary & tertiary insurance.
-
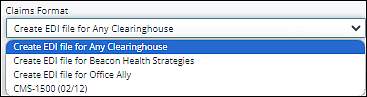
Claims Format Drop-Down Options: selects between the production of paper claims or electronic claims
- CMS-1500 (02/12) - creates a paper claim in PDF format
- Submit automatic EDI file - formats and sends claim to clearinghouse
- PDF Settings Button: adjusts how a PDF generates. See Claim Margin Alignment PDF Settings article for more information
- File Type Radio Buttons: selects whether claims will be created in a test or actual production format
Clear Button: this button will negate all selections made above it and clear all fields
Create Claims Button: this will create your claims in either paper or electronic format, depending on the choice made in the Claims Format.